Chapter 9
Effects of the Sun, Maladies, etc.
The #1 Threat
My Travel Clinic
Self-Diagnosis
Playing Doctor
Maladies
Items of the Colon
Food Poisoning
Rehydration Therapy
Women's Concerns
AIDS
Insects...Urine Fish
Mosquitoes
Wounds, Rashes
Foot Care
Effects of the Sun
Cold and Frostbite
Altitude Sickness
Jet Lag
Medical Kits
Returning
Home Tips
IN NORTH AMERICA, Europe, Australia, New Zealand, South Korea, Japan, and a few other
places your most likely health problems are foot blisters, colds, constipation, and
hangover. In the rest of the world most travelers are likely to encounter nothing more
than mild diarrhea from unfamiliar microbes introduced into the intestines.
Don't allow fear of health problems forestall developing world travel--if you sit at
home you might have a heart attack or develop a horrible disease of the ass! While
headline-grabbing diseases such as Ebola, Lassa Fever, and plague are terrifying,
travelers don't get them. These are diseases of grinding poverty and
ignorance. For twenty years we of the developed world have been suffering the
deadliest and most insidious virus of all--so try to maintain perspective.
With the sensible precaution of seeking and following advice from a travel clinic your
health risks are greatly reduced, as most risks are directly related to awareness. You
don't want to be as naïve as I on my first backpacking trip into the developing world.
(See photo below and Drinking Tips in Chapter
21.)
 |
Photo: Here I'm feeling chipper
compared to a few hours earlier. Note the language dictionary in my right hand--the doctor
spoke English, the nurses did not. Many thanks for the wonderful care from
all. |
By far the greatest threat to the traveler is being run over by a moving vehicle, or
from a crash while in a moving vehicle. Even for Americans on comparatively safe American
roads there is about a one in one-hundred lifetime chance of perishing in an automobile
accident, and many times that for serious injury.1
Therefore the most important steps for traveler safety are obvious--always wearing a
seat belt or helmet, always looking both ways before crossing a street, and standing well-back from
the curb. Keep this in mind as you read about malaria, cholera, and urine fish.
Driving in Developing Countries and Remote Areas
(Chapter 21 Considerations)
From a March 1997 email (bottom)
Sources For Current Information
If planning a journey to the developing world, this chapter will not provide
all the information you need. That information is not available in any book, as epidemics
and outbreaks occur and change much too quickly. Constantly updated information is
available from:
Centers For Disease Control, Atlanta, Georgia (voice tel. 404-332-4559 fax-back
888-232-3299)
cdc.gov
The CDC webpage is used by travelers from everywhere for the latest worldwide disease
and health information. You can also listen to exhaustive recordings of health information
over the phone by requesting specific topics via touch tones, or use their fax-back
service. Many travel clinics receive software updates from the CDC, and provide that
information to customers, one of which you should be before and after developing world
travel.
Most major cities have a private or public travel clinic to assist international
travelers with preventive measures, and to treat diseases brought back. After being
pitifully laid out and hospitalized on my first tour into rural Mexico due to stupidity,
there was no question that before my next journey into the developing world I would seek a
travel clinic and spend whatever necessary to get fully immunized, as well as medically
and mentally equipped.
Soon I had the opportunity for a few months in Central America, so I made an
appointment with the Travel Clinic in Austin, Texas. During the initial $45 visit a
knowledgeable Registered Nurse discussed my case. She also had access to a computer file
from a private company called Travax, which was a compilation of information from the CDC
and the State Department. It was updated weekly.
I was given forty pages of useful computer printout on eight Central American
countries. Topics for each country were AIDS, cholera, malaria, hepatitis, polio, rabies,
typhoid, yellow fever, cholera, insect-borne diseases, food and water-borne diseases,
testing requirements, and a general description of each country. Most eye-opening were
U.S. Department of State travel advisory reports, including descriptions of recent
criminal activity against travelers, warnings about possible drug penalties, assessments
of medical facilities, and embassy locations and phone numbers.
On my first visit to the clinic I received a polio booster shot in one arm ($25) and a
tetanus-diphtheria (Td) booster shot in the other ($15). Both arms were slightly sore at
the place of injection for two days.
I was given prescriptions for chloroquine, Cipro, and a Typhoid oral vaccination.
Chloroquine is an anti-parasitic drug which usually kills malaria-causing protozoa in the
blood. It is taken once weekly beginning one or two weeks before entering an infected
area, and for four weeks after leaving an infected area. I bought the generic chloroquine
for about $2.50 per capsule--$1 less than the brand name.
Cipro is a brand of ciprofloxacin antibiotic available through prescription. It is
effective against travelers' diarrhea since it causes fewer side effects than
broader-ranging antibiotics. Recommended dosage was one 500 mg tablet twice per day for
three days. Cost was $20 for six tablets, but I bought twelve as Cipro has a long
shelf-life, and I knew from experience how vital an effective antibiotic could be.
I was instructed to carry Cipro, Immodium, and a thermometer. If I contracted mild
diarrhea, which was defined as several bowel movements per day while feeling fairly well, no
treatment was indicated. If the diarrhea was severe I was instructed to check my
temperature. If it was above normal I was to take 500mg of Cipro twice per day for three
days. If my temperature was normal, I was to take the Cipro as above, and to take
one Immodium tablet four times per day for three days.
The reason for not taking the Immodium while running a fever is that fever may indicate
organisms in the bowels which are likely to invade the intestinal lining. Since Immodium
slows intestinal movement (plugs you up), it would allow the bad bacteria a better chance
to invade the lining and prolong diarrhea.
I was also told to seek medical help if self-treatment did not work, and if there was
accompanying high fever, blood, or mucus in the stool, which are all indicators of
infection.
The Oral Typhoid Vaccine cost $42 and consisted of four capsules to be taken with cool
water one hour before meals every other day. Since this was a live vaccine the capsules
had to be kept cool. I was given an ice-pack for transport home. This oral vaccine was
said to have fewer side effects than the injectable version.
About ten days later I returned to the Travel Clinic for an immunoglobulin
(gammaglobulin) injection ($9) in the hip, and a yellow fever vaccination ($52) in one
arm. The immunoglobulin shot contained antibodies to combat Hepatitis A, which provides
some protection for up to five months. It should, however, be taken as close to departure
as possible to ensure maximum effectiveness. The yellow fever shot is effective for ten
years.
After this second visit to the Travel Clinic I had a very slight fever and chills, and
was slightly tired for a few days. This was considered a normal reaction. My hip
definitely ached from the immunoglobulin shot.
Find a travel clinic in your area by checking the yellow and white pages under Travel
Clinics, or by calling your local public health agency, hospital, or doctor.
International Health Certificate (Yellow Card)
This card documents your immunization history. Required for entry to some countries for
proof of yellow fever inoculation, it is available from travel clinics, and possibly your
doctor. It's yellow.
Travel Health Insurance
Many companies sell travelers' health insurance for one to several dollars per day.
Usually you pay the medical costs while abroad, but are reimbursed upon return. More
expensive plans pay for emergency air transport home.
If you already have health insurance check if your current plan provides coverage in
other countries. There's a good chance it does, though it probably won't cover emergency
air transport.
ISIC (International Student Identity Card) holders get coverage with the card. Other
plans are available from many travel agents, including Council Travel and other
budget/student specialists. Search the web or see Chapter
23-b Useful Information for a dozen companies that offer travel insurance.
Some European and other advanced countries with national health systems treat--at no
charge--travelers from other countries on a reciprocal basis. Citizens of the United
States, of course, are on their own.
The knowledge base doctors use to diagnose is a thousand times greater than the
following list of symptoms and disease characteristics. Don't try to diagnose yourself or
someone else--seek professional advice as soon as you can. Even in developing countries
where doctor training may not be extensive (in Mexico I was superbly treated by a
twenty-two-year-old), they will be familiar with local health problems.
Another point is that treating yourself with too few or the wrong antibiotics can be
seriously unhealthy. The wrong antibiotics can facilitate germ entry into new areas of the
body, while too few might allow the infection to spring back worse than before.
Learn from my mistakes!
- You may not notice a slightly elevated rate of breathing, or if you do, you may not
connect it with rapidly developing pneumonia. You may also be fooled (not that you have
any knowledge or experience to fool) because the patient's symptoms (temperature,
vomiting, etc.) appear (to you) to be improving. The situation can suddenly change for
much worse or disaster due to something under the surface of what untrained and
inexperienced eyes can see.
- "What's going around" may have relevance in a macro sense, but it may also
have little or nothing to do with your patient/friend/loved one due to age, health,
medication, etc.
- Don't put too much stock into advice over the phone (unless it's to seek professional
help right away), even if it's from a good source. The difference between a description by
someone with nearly zero experience and the patient being seen by a medical professional
is like night and day.
- Many lives could be saved and much suffering avoided if people who basically don't know
anything (unless you're a doctor or nurse, that's you!) would get successively wiser, more
experienced, better educated, better trained hearts and minds involved to help think and
make decisions. This should be done in minutes or hours, not days.
- Get her the best trained, best equipped, and most compassionate care available. While
this must be balanced with time/distance/transport factors, it's probably wise to go
sooner for the superior care.
- If you are the patient, don't downplay your symptoms. The doctor needs to know exactly
how it is so he can make good decisions. In one case the patient kept telling the doctor,
"It's probably nothing, I'm okay," etc., when in fact he was having a major
heart attack with a lot of pain!
- It can be especially difficult if you normally rely on the patient/friend/loved one for
decision-making help, but the patient is too sick to provide reasonable guidance. Seek
professional medical help right away!
- You must act to preserve life, ease suffering, and increase joy by properly valuing your
patient/friend/loved one as early as possible, and by getting professional medical help as
soon as possible.
Maladies of Interest to Travelers
The following is a concise overview of major threats facing travelers. I hope it
encourages you to seek professional medical advice from a travel clinic before visiting
the developing world.
Most of this information came from the CDC, my travel clinic, the American Medical
Association Encyclopedia of Medicine, several travelers' health books, and my limited
experience. While I have tried to be accurate and informative, please
understand that I am
writing outside my fields of expertise (travel gear, hitchhiking, women), that I am neither a doctor or nurse, and that the best and only course of
action is to see a medical professional.
- Colds
- are common among travelers. One had five over six months in
Europe. He was also drinking more alcohol than usual, and not eating well. Because there
are over two hundred viruses associated with colds, those prevalent in Europe or China may
quickly overwhelm your immune system.
- Since colds are transmitted primarily by direct contact, incidence is reduced by washing
hands, especially before eating, and by keeping fingers away from the face. Colds
gain initial foothold in mucous membranes, so drink plenty of fluids to keep them in
good shape.
-
- Diphtheria
- is very rare in developed countries due to widespread use of the Td vaccine, but
is
still endemic in poor, developing countries, and a hazard to non-immunized travelers.
There is currently a diphtheria epidemic in the countries of the former Soviet Union.
-
- Diphtheria is an acute (suddenly developing) bacterial illness which causes a sore
throat and fever, and can be life-threatening when the bacteria release a toxin into the
bloodstream. About ten percent of victims die. Prevention is by updating your Td
vaccine.
- Tetanus
- is also called lockjaw. 500,000 cases develop annually worldwide, but only about one
hundred in the U.S. due to widespread immunization with the Td vaccine. While a booster is
recommended for the general population every ten years, the vaccine's effectiveness falls
off enough that if you get a major cut or puncture between years five and ten, it's
apparently standard practice to get another booster. (Hence I'll get a booster every five
years for developing world travel.)
- Symptoms include stiffness of the jaw, back, and stomach muscles, and a contraction of
facial muscles. Wounds should be thoroughly cleaned and an antiseptic applied. Tetanus is
serious and sometimes fatal. Prevention is by the Td vaccine.
- Diarrhea
- is often contracted by visitors to the developing world for a few days. It is generally no
great problem, and the discomfort usually lessens after a day or two.
- Diarrhea is most often caused by unfamiliar bacteria. Mexicans
traveling in the U.S. sometimes get Uncle Sam's Revenge. Anxiety is also a
precipitator.
- It's best to let normal diarrhea run its course, which takes two to five days.
Drink plenty of liquids to flush-out your system, and to avoid dehydration. Eat no solid
foods on the first day. On the second day begin eating bland foods such as toast, soup,
rice, and bananas.
- If you need to plug your system for a day so you can travel, the over-the-counter
drug Immodium works safely and well. The active ingredient in Immodium is loperamide,
which is also used in several other medications. Do not use loperamide for extended
periods as the intestines must be cleansed naturally. Loperamide doesn't cure anything.
- Many travelers swear by Pepto Bismol tablets for soothing the stomach and easing
diarrhea. I usually have these tablets in my pack, and when traveling developing
countries, several in my wallet. Pepto Bismol turns your stool a dark black.
- Dysentery
- is a severe infection of the intestines, characterized by passage of mucus and blood. It
has two forms: bacillary and amebic. While both are prevalent in many developing
countries, they are rare in travelers compared to simple diarrhea.
- Bacillary dysentery
- is also called shigellosis, after the shigella bacteria which cause it.
Bacillary means "rod shaped," which describes the bacterium. The usual source is
from infected food handlers failing to wash hands properly, and from flies landing
on food after having been somewhere nasty.
- Symptoms begin one to four days after infection, and are characterized by a sudden
onslaught of watery diarrhea, abdominal pain, vomiting, nausea, and fever. After several
days blood and mucus begin passing. It is highly contagious.
- Treatment consists of rehydration therapy. Solid food should not be eaten for the first
day or two. Antibiotics may be useful. Most victims begin recovering after about a week.
Babies, children, and old people risk death due to dehydration.
- Amebic dysentery
- is also called amebiasis, from the single-celled ameba (smallest animal)
parasite entameba histolytica. Amebic dysentery results from swallowing the
histolytica cysts via infected water or food (especially beware lettuce, uncooked vegetables, and
unpeeled fruit). It is found in the same areas as bacillary dysentery.
- Symptoms range from a few loose stools with rumbling pains in the stomach, to a severe
case with high fever and bloody, watery diarrhea. It comes-on slower than bacillary
dysentery. It can cause shaking chills, fever, weight loss, and painful enlargement of the
liver.
- Treatment is with rehydration therapy and amebicide drugs such as metronidazole, which
effect full recovery within a few weeks. It won't go away on its own like bacillary
dysentery.
Prevention for both types of dysentery is by eating only cooked vegetables and peeled
fruits, and by only drinking boiled or purified water.
I use the term food poisoning for three intestinal wars that for some reason went far
beyond the mild discomforts of travelers' diarrhea. Indeed I feel lucky to have survived.
The first is described in Drinking Tips in
Chapter 21. The second occurred on the last half of a three day bus journey after
mindlessly gobbling an apple purchased through a window and kindly presented by a fellow
passenger. While that was inconceivably stupid after months of incident-free travel in
very poor countries, I wasn't without luck. The bus was only half full and--miracle of
miracles--it had a working toilet.2
The third war played out in my apartment thanks to a now discontinued salad from an
American fast food restaurant.
While I can only describe the agony and weakness as nearly complete, here are a few
points should you find yourself in a similar situation.
1) Seek medical help if at all possible. Serious food poisoning
often kills, especially the young, the old, the weak, and those with pre-existing
conditions.
2) There may be a warning or premonition of your impending fate, so
take action while you can, such as:
- Notify someone, especially of authority
- Get to, or closer to, a doctor or clinic
- Make available lots of clean water or other nonalcoholic liquids
- Secure the best available environment
- Anything you'll be glad to have done in the few minutes you'll be lucky to have
3) After the initial wave of expurgations and you're well into
the dry heaves, drink clean fluids even when they soon come back up. This cleanses the
system faster, and the ten percent that is absorbed staves off dehydration. While clear
liquids are often recommended, I prefer any soft drink for extra energy and superior taste
in both directions.
4) Don't plug up your back end with drugs. The toxins must get
out. Pepto Bismol may help later.
5) Riding a speeding bus toilet for hours or days is supremely
unhealthy--better to get off when possible.
6) Flush, cover up, or crawl away from the horrific stench
immediately. Open vents to avoid explosion. (Or, 1. ...how the
driver was able to maintain consciousness. 2. If Sadaam should ever...)
7) Pray for God's help!
|
-
- Cholera
- results in severe water loss due to watery diarrhea and vomiting. The cholera bacterium
produces a toxin which increases the passage of fluid in the bloodstream to the
intestines. Death can result in a few hours from rapid fluid loss. Infection is by
ingesting food or water infected with the bacteria, but especially from shellfish. In two
hundred years cholera has spread from northeast India to most of the developing world,
including South and Central America, and Mexico.
- While the risk of cholera to travelers is slight, in 1993 in Guatemala City I read a full-page newspaper article about a
cholera outbreak/scandal in Chiquimula, a thriving middle-class city I had visited the
previous week. Water works employees had failed to chlorinate the water, and four hundred
people had come down with cholera, killing eleven.
- Symptoms begin one to five days after infection, and include diarrhea and usually
vomiting. Treatment consists of immediate rehydration therapy to prevent dehydration and
death. Ninety-nine percent of victims recover given adequate rehydration.
- Prevention consists of drinking only bottled or boiled water, and taking as much care
with food as possible. A vaccine is available, but is only about fifty percent effective
for three months. My travel clinic did not recommend the vaccine due to its
ineffectiveness, expense ($45), and the rarity of cholera in travelers. Other backpackers
have taken the vaccine because they were told it might reduce symptoms.
-
- Constipation
- is common due to the change in routine and diet. Make a point to drink plenty of fluids,
and eat roughage. Fighting has been reported in England over lettuce. Otherwise a pint or
two or three of Guinness provides relief.
Rehydration therapy is urgent in case of dehydration, usually due
to severe diarrhea and vomiting. It is especially crucial for infants and old people who
have suffered rapid water loss. Dehydration from diarrhea is the leading baby killer in
many developing countries. The two types of rehydration therapy are intravenous, performed
with a salt/sugar/water solution in the hospital, and oral, which can be done anywhere.
Oral rehydration solution consists of:
water: 1 quart or 1 liter
salt: 1/2 level teaspoon
sugar: 8 level teaspoons
sodium bicarbonate (baking soda): 1/4 teaspoon
The sugar aids absorption of the water and salt. Sodium
bicarbonate isn't necessary if unavailable. Be careful with measurements as too much salt
can increase dehydration. Dispose of unused solutions after twenty-four hours since
bacteria may multiply. Patients should drink more solution as able. A gallon or more may
be needed. Commercially prepared solutions to which you just add clean water are available
from pharmacies. It tastes vile, but you have to force yourself to drink it.
|
-
- Hepatitis type A
- is also called infectious hepatitis, and is the most common serious disease
among travelers in the developing world. Type A is transmitted by a virus through fecal
contamination, again via food or drinks prepared by an infected person with poorly washed
hands. While it is found worldwide, travelers are most susceptible in developing countries
with low food handling standards.
- Symptoms are either nonexistent or abruptly begin two to six weeks after exposure. They
resemble the flu, including fever, aches, loss of appetite, nausea, abdominal discomfort,
and liver pain (on your right side). Urine may darken, and stools may become lighter and
yellowish. After four to seven days the symptoms may become more severe, including
diarrhea, vomiting, itching, and jaundice. Skin and whites of the eyes may turn yellow.
Most recover within six weeks. Hepatitis type A does not lead to chronic hepatitis.
- There is no treatment for hepatitis A. Victims must rest and abstain from alcohol until
they recover. This recovery of the liver so weakens the victim they often can do no more
than hole-up in a fleabag hotel, or swing in a hammock under a palapa twenty hours per
day. Prevention is by taking care what and where you eat. An immunoglobulin shot provides
some protection for up to five months, the Havrix vaccine for up to ten years.
- Hepatitis type B
- is also called serum hepatitis. It is found in the blood, semen, and other body fluids
of infected persons. It is spread in the same manner as AIDS (sexual contact, IV drugs,
and infected blood products). Type B is found worldwide, but is much more prevalent in
Asia and Africa. Symptoms, when they occur, are the same as for hepatitis A, except
sometimes more severe. Many people are completely symptomless.
- About ten percent of hepatitis type B cases lead to chronic hepatitis, which is a severe
inflammation and destruction of cells within the liver. This leads to cirrhosis.
- Prevention is with the hepatitis B vaccine, although this is usually only recommended
for health care workers, people who have many unprotected-sex partners, and drug addicts.
Immunoglobulin
Immunoglobulin is also called gammaglobulin. It is a human plasma
product containing antibodies against measles and hepatitis A. Immunoglobulin is highly
recommended by the Centers for Disease Control for travelers staying at least three weeks
in areas of suspect hygiene and sanitation. It offers some protection for up to five
months. Since this protection fades with time, it is best to receive an IG shot just
before traveling to developing nations.
Immunoglobulin is composed of blood products, which in the U.S.
are screened for HIV and other diseases, rendering it safe, according to the CDC. Since
other countries may have shoddy or nonexistent screening, the CDC strongly advises not
getting immunoglobulin elsewhere. I would expect the odds of shoddy or nonexistent
screening for the U.K., Canada, Sweden, Germany, etc. would be the same or less than the
U.S., but that's a guess.
Havrix
A vaccine for hepatitis A called Havrix was introduced to the American market
in 1996. (Other brands were available in Europe for several years previously.) It requires
a booster after a year and is expensive at about $100, but offers more protection than
immunoglobulin and lasts up to ten years.
Consult with your doctor, of course, but the vaccine is probably worth the money as a
bad case of hepatitis A can seem Sisyphean at the very time you'd most prefer to be
healthy, and going back for IG shots is no fun.
|
-
- Typhoid
- is caused by the bacteria salmonella typhi. Feces, urine, and contaminated food and
water are the principal sources of infection--again often through a food handler with poor
hygiene. Sewage-contaminated shellfish is also a source.
-
- Most symptoms are limited to a fever of one week, but can include headache, anorexia,
general malaise, and constipation, giving way to diarrhea, a non-productive cough,
nosebleed, and raised pink spots on the upper abdomen. Complications may result, and the
death rate for serious cases is ten percent for those untreated, one percent for those
treated.
- Treatment is with antibiotics. Prevention is by cautious eating and drinking, and by an
oral or injectable vaccine, both of which are about sixty-five percent effective for five
years. The oral vaccine is four pills taken every other day; the injectable requires two
shots one month apart. The oral vaccine has lesser side effects.
- Antibiotics are not recommended as a preventive since they disrupt normal intestinal
bacteria and can facilitate infection with salmonella typhi.
- Polio
- is a viral disease which has been virtually eliminated in the developed world, but is
still a threat to non-vaccinated travelers in developing countries. Some beggars in
developing countries with wasted feet and legs are polio victims. There is no effective
treatment for polio. Prevention is with either the oral or injectable vaccine.
- Malaria
- poses the greatest health risk to travelers in warm climates, and is in fact
the greatest health threat to humanity. Up to 300 million cases occur worldwide each year,
with about one million deaths in both Africa and Asia. The tragedy is currently increasing
as mosquitoes become insecticide-resistant and forms of malaria become drug-resistant.
- Malaria is spread by the bite of the Anopheles mosquito, which generally feeds dusk
through dawn. It is caused by four types of a single-celled protozoa: vivax, ovale,
malariae, and falciparum. These parasites attack and explode red blood cells.
- Symptoms for the first three types may include the classic malarial fever, which is
called an ague (pron. ae gyoo). This occurs in three stages which rhythmically
coincide with millions of parasites being released into the bloodstream after bursting out
of red blood cells. First is a cold stage characterized by severe shivering, followed by a
high fever stage of up to 105º F (40º C). Finally there is intense sweating which brings
the fever down. The victim may also vomit and have a bad headache. The patient is left
weak and tired, and sleeps.
- These stages may occur cyclically, either every other day or every third day, but only
after the disease is well-established. Malaria can be very difficult to diagnose in
early stages.
- Falciparum is a more severe type of malaria as all red blood cells are
attacked. Death may result a few hours after symptoms begin. The brain may be affected,
and liver and kidney failure are common.
- Treatment is usually with a big dose of chloroquine. Falciparum malaria is resistant to
chloroquine, however, so other drugs must be used. Discuss treatment with your travel
clinic before you go, and immediately with local medical professionals if you acquire
malaria-possible symptoms.
- Malaria prevention is complicated, so only trust a high quality travel clinic to
prescribe the proper medications for your specific destinations and singular physiology.
-
- Chloroquine (brand names Aralen, Avloclor, and Resochin) should be
taken weekly beginning at least one week before entering a malarial area, and continuing
four weeks after leaving. Beginning the regimen two weeks before departure is often
recommended so there will be time to change medication in case of reaction. It's
traditional to take chloroquine--and to remind other travelers to do so--on Sunday.
- In falciparum malarial areas, such as Panama east of the canal, a weekly dose of
mefloquine (brand name Lariam) may be prescribed. Three tablets of
sulfadoxine/pyrimethamine (brand name Fansidar) may be prescribed to be taken
immediately if flue-like symptoms suddenly develop. Some people have severe skin reactions
to Fansidar, and various neurological, psychiatric, and flue-mimicking symptoms
have been ascribed to Lariam.
- Chloroquine and the other anti-malarial drugs are not vaccines, and they do not
guarantee immunity from infection. They are prophylactic medications--taken properly, they
usually suppress and prevent malaria. Thus most travelers who take the proper
medications, use DEET insect repellent (detailed below in How to Avoid
Insect Bites), wear long sleeves and pants, and drape mosquito netting around their
beds don't get malaria.
- Yellow fever
- is a viral, hemorrhagic (bleeding) disease transmitted in urban areas from person to
person by Aëdes aegypti mosquitoes, which feed during the day. In jungle areas it is
transmitted from monkey to man by various mosquitoes. Yellow fever is found east of the
Panama canal, in parts of South America, and in much of Africa.
- Symptoms begin three to six days after infection, are relatively mild in eighty percent
of cases, and include fever, headache, and weakness, which last up to four days. The other
twenty percent are more serious, including high fever, chills, nausea, vomiting, bleeding
from the gums and nose, and severe pain in the neck, back, and legs. These may last a few
days, followed by a remission, and then followed by a more severe illness, including
increased fever, vomiting of blood, and jaundice due to liver damage--hence the name
yellow fever. Approximately five percent of all victims die within days of symptom-onset.
- Treatment consists of maintaining blood volume and fluids. No drug works against this
virus.
- Prevention is by the yellow fever vaccine, which lasts ten years. A yellow fever
vaccination certificate (yellow card) is required for entry into and from countries where
the disease is prevalent.
- Dengue fever (pron. den gay)
- is also called breakbone fever after the debilitating pain it causes. It is another
viral, hemorrhagic disease transmitted by day-feeding Aëdes aegypti mosquitoes, and thus
found in tropical and subtropical regions worldwide. While I was in the Petén region of
Guatemala an epidemic of dengue was ravaging the local population.
- Symptoms appear five to eight days after a bite from an infected mosquito, and include
high fever, severe muscle and joint pain, and rash. They subside and recur about every
three days. Recovery takes several weeks, with victims rarely dying.
- Treatment is with pain killers to relieve symptoms--there is no specific
treatment.
-
- Prevention is, as always, by avoiding mosquito bites. There is no vaccine.
- Chagas' disease
- is also called American sleeping sickness, and can be fatal. It is transmitted by the
bite of the assassin bug, which makes its home in thatched roof and adobe huts in rural
Central and South America, but especially Brazil. This bug prefers to bite on the
face
and defecate. Single-celled parasites called trypanosomes enter the body, grow to
huge numbers, then attack many organs, including the heart. Diagnosis is by a hard, purple
swelling which appears on the bite site about a week later.
- Treatment is effective only if caught early.
-
- Prevention is by not sleeping in mud huts, by using mosquito netting, or by at least
sleeping in the middle of the room away from walls. This disease is extremely rare in
travelers.
- Plague
- is transmitted to humans by the bites of rodent fleas. While a few cases of plague occur
every year in the American Southwest, it is mostly a disease of South America, Africa,
Southeast Asia, and India. Plague is the "black death" that repeatedly wiped-out
Europe during the middle ages. The risk of plague to travelers is almost zero, especially
if you make a habit of not handling rats, dead or alive.
- Rabies
- is also known as hydrophobia, and is an acute viral disease of the nervous system. Almost
invariably fatal if left untreated, it is transmitted by animal bites, scratches, or even
licks on an open cut. There are about 30,000 deaths every year from rabies, nearly all in
developing countries.
- Skunks, raccoons, and bats are the major carriers in North America. In Central and South
America dogs and vampire bats are the primary vectors. Rabies is fairly common in some
areas. Stray dogs are numerous, and vampire bats are a threat to those sleeping outside
without mosquito netting. A vampire bat lands near a sleeping mammal, creeps up, and
delivers a painless bite with razor-sharp teeth. It then laps up the blood, which doesn't
coagulate due to inhibitors on the tongue. Horses and cattle are the usual prey, not
backpackers. Any bat found on the ground is quite possibly a rabies victim. Do not touch
it.
- Jackals are the primary carriers of rabies in Africa. In Southeast Asia and India dogs
are the leading vectors to humans. Note, however, that any mammal bite may transmit
rabies.
- Ireland, Britain, Norway, Sweden, Japan, Australia, and New Zealand do not have the
disease, and require an extensive quarantine for pets entering the country.
- Symptoms of rabies begin from nine days to many months after exposure. These include
fever, hyperactivity, seizures, and often an intense thirst that cannot be quenched since
liquids produce violent and painful spasms in the throat. The victim will die within three
to twenty days from onset of symptoms.
- Prevention and treatment is through passive immunization before
symptoms
appear, and ideally within two days of exposure. Competent medical advice should be
immediately sought after a bite in a rabies endemic country. (Not a snake doctor.) Clean
the wound thoroughly with soap and clean water for at least five minutes, but don't stitch
it closed. The sooner vaccination is begun, the better the prognosis. Today's vaccines are
not so painful, and are no longer given through the stomach.
- Brucellosis
- is a rare bacterial infection in the U.S., but travelers who drink unpasteurized dairy
products in Latin America and Mediterranean countries may be at risk. Symptoms include
high fever, shaking, sweating, and severe depression. Treatment is with antibiotics and
rest.
- Schistosomiasis (bilharziasis)
- is common in tropical regions worldwide, affecting about 200 million people. It is
caused by several species of flukes (flattened worms) called shistosomes. They live in
fresh water lakes and rivers, where they live part of their life cycle in snails.
- Symptoms vary from none to serious. The first is usually an itchy rash where
the parasite has burrowed through the skin. Weeks later flu-like symptoms may begin,
including high fever, chills, muscle aches, and diarrhea. The symptoms may go away and
recur a month or two later. Long-term damage includes cirrhosis and kidney failure.
- Treatment is with a single dose of an anthelminthic (antiparasitic) drug, which kills
the flukes. Prevention is by avoiding freshwater rivers and lakes in the tropics, but
especially the Nile Valley, where schistosomiasis is rife.
- Leishmaniasis
- is a variety of diseases caused by a single-celled parasite transmitted via sandfly
bites. Some varieties affect mostly the skin, producing large ulcers at the bite area. In
the Middle East this is known as the Baghdad boil. South American forms of the disease may
cause more severe tissue damage, especially to the face. Another variety, called kala
azar, causes internal organ damage.
- Treatment is effective with sodium stibogluconate. Prevention is by avoiding sand fly
bites by wearing shoes, socks, pants, long-sleeves, and by using DEET.
- Filariasis
- is a variety of tropical diseases caused by larvae or worms, and transmitted to man by
insects. These diseases include the childhood bugaboo elephantitis, which causes
enlargement and hardening of arms, legs, and scrota, and onchocerciasis, below.
- Onchocerciasis (river blindness)
- is caused by a worm infestation in Central and South America, and Africa. The parasite
is transmitted from person to person by the black simulium fly, which is found only near
fast-moving rivers and streams. Up to twenty million people are affected, causing
blindness in many. In some African villages fifty percent of the old people have river
blindness.
- Treatment is with the drug diethylcarbamazine, which must be administered under close
medical supervision since severe reactions to the dead and dying worms may occur.
Prevention is by avoiding black fly bites.
- Giardiasis (beaver fever)
- is the bane of wilderness backpackers in the United States. It is also found worldwide,
especially in the tropics and the public water systems of the former Soviet Union. It is
an intestinal infection caused by a single-celled parasite. Wilderness backpackers in the
U.S. must treat all water, even from crystal clear brooks in Yosemite, due to the
prevalence of this organism.
- Giardia cysts (eggs) are spread from the feces of infected animals. The cysts hatch two
or three weeks after ingestion, causing abdominal symptoms such as violent diarrhea,
foul-smelling gas, and cramps. Sixty percent of those infected, however, show no symptoms.
Giardiasis clears up on its own after two or three weeks, although metronidazole speeds
recovery.
- Prevention is by drinking only pure or treated water.
Women's Concerns
- Cystitis
- is a common infection of the urinary tract and bladder among
travelers. The main symptom is a frequent urge to urinate, accompanied by burning
or stinging. The amount of urine passed is usually small, and the pain can be great.
Cystitis is sometimes associated with sex, and symptoms are similar to several sexually
transmitted diseases which can lead to infertility and cancer if not properly treated.
Therefore a doctor must always be consulted.
-
- Treatment is with an antibiotic to eliminate the infection and
prevent it from spreading to the kidneys. Drink large quantities of liquids, especially
cranberry juice, to speed recovery and as a possible preventative.
-
- Initial pain can be relieved with the urinary tract analgesic
phenazopyridine hydrochloride, available through prescription (Pyridium) or over
the counter (ask a pharmacist). This is a pain reliever, not an infection fighter, so
again, a doctor must always be consulted, perhaps especially if symptoms seem to
go away on their own.
- Vaginal infections
- Tropical climates and taking antibiotics for diarrhea and other
ailments may increase incidence, which may be reduced by wearing light, loose
clothing, and cotton underwear instead of nylon.
- Pregnant
- women should consult their doctor before traveling to developing
countries. Some vaccinations, antibiotics, and antimalarials may be harmful to the fetus.
Nearly 20,000 people are infected every day.
The hardest hit area is sub-Saharan Africa, where AIDS is called "slim" due
to its wasting effects. In some areas up to twenty percent of the population are carriers,
as well as nearly all prostitutes. In Africa AIDS is spread primarily through heterosexual
sex. The blood supply in Africa is likely to be poorly screened, if at all, so you must
avoid transfusions. Travelers in Africa should bring their own hypodermic needles for
emergencies.
AIDS is also spreading rapidly in Asia, again primarily through heterosexual contact.
Since the epidemic became widespread there only a few years ago, deaths are still rare.
Thailand is the main foci, with a significant percentage of prostitutes infected. In 1996
over three million cases of HIV (the virus that eventually causes AIDS) infection were
estimated in India--this number will mushroom.
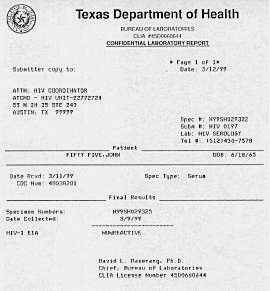
| Many countries now require HIV testing for long-term visitors of greater than six
months, or applicants for work or residency. In most cases HIV testing is not required for
visitors of a few months or less.
As you travel remember that most HIV carriers--whoever they are--don't know they're
infected, and HIV is thought most infectious the first year after infection.
|
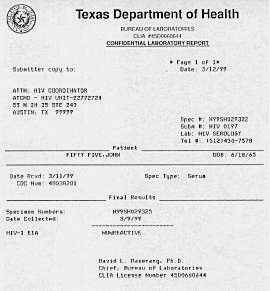
|
| Perspectivizer--get one today. |
Insects, Worms, Single-Celled Animals, and Urine Fish
- Jiggers
- are also called burrowing fleas, and are a type of sandfly found in tropical areas of
the Americas and Africa.. They burrow between toes and under toenails, where eggs are
deposited under the skin. Symptoms are a painful and itchy pea-sized swelling. Treatment
is by removing the jigger with a sterile needle, and thoroughly cleaning with antiseptic.
Prevention is by wearing shoes or at least sandals, and by keeping nails well-trimmed.
- Chiggers
- are found worldwide on grass and weeds. These red mites attach themselves to bare legs
and ankles and feed on blood. They may cause a painful, itchy swelling about a half inch
in diameter. Prevention is by wearing socks and pants, and by applying DEET to exposed
skin, socks, and pant cuffs.
- Bedbugs
- are small, flat, usually brown bugs. They live in beds and furniture during the day, and
come out at night. Bedbugs often leave a straight line of red bites across the skin. They
rarely spread disease, but the bites should be cleaned with antiseptic to prevent
infection. Avoid bedbugs by checking bedding carefully--look for tiny red splotches on
sheets and blankets. If you see their sign, take another room or string-up your hammock.
 |
Left: These are large black ants. The
column is about a foot wide. |
 |
|
Right: Here large red ants rampaged a 20 by 20 foot area, attacking and
devouring insects across the jungle floor. Very interesting to watch. They ignored me. |
- Sandflies
- are tiny, nearly-invisible long-legged flies common to tropical areas. Sandflies can
transmit several diseases to humans, including leishmaniasis, bartonellosis (in the
Andes), and sandfly fever.
- Since sandflies are most active at dawn and dusk, walking at those times stirs them up
and results in numerous, amazingly irritating bites. You won't be bothered as much if you
sensibly remain in, or retreat to, your hammock during dawn and dusk. Also cover exposed
skin, especially legs, ankles, and arms, and use DEET. Socks help a lot.
- Lice
- are tiny, flat, wingless bugs. Body lice are killed by washing clothes in very hot
water, or by using a hot dryer. Head and pubic lice can be killed with lotions and
shampoos containing benzene hexachloride.
- Scabies
- are tiny mites that burrow into the skin, lay eggs, and cause intense itching,
especially at night. Treatment is with an insecticide lotion.
- Hookworms
- are half-inch long worms that live in the small intestines of 700 million people
around the world, especially in the tropics. They have hook-like teeth. Their life cycle
begins with larvae burrowing into the feet, or by ingestion. A large infestation of
several hundred hookworms may eat several ounces of blood per day, causing anemia.
- Symptoms, called ground itch, may include a red and very itchy rash on
the feet that lasts for several days. A cough and pneumonia are also possible when a heavy
infestation passes through the lungs.
- Prevention is by wearing shoes or sandals. Treatment is with an anti-worm drug.
- Guinea worm
- is the "fiery serpent" scourge of the Biblical Israelites. It
is an up-to three-foot long female worm that now plagues eighteen African and Asian
countries, although recently eliminated from Pakistan. Infection is by drinking water
containing the cyclops crustacean water flea.
Symptoms begin a year later when the worm
is fully grown and ready to reproduce. It comes to the surface of the skin where a blister
forms. Hives, diarrhea, and vomiting often occur at this time. When the blister bursts the
end of the worm is exposed, and debilitating pain begins.
The traditional treatment is to wrap the exposed worm around a stick, and then gently
wind it out over several days. This is dangerous (although impressive) as the worm can
break and an infection develop.
As guinea worm must live part of its life cycle in man, it is only the second disease
(after smallpox) targeted by the World Health Organization for eradication, aided by great
diplomatic imprimatur from the Carter Center.
- Beefworm (botfly larvae)
- is the only creature known to penetrate my defenses in Central America. It is common in
the jungles of Belize.
- The botfly is an ordinary-looking fly with unusual child-rearing habits. It captures a
mosquito in flight and lays eggs on it. The mosquito is released, and when it subsequently
bites a warm-blooded prey some of the eggs fall off and are hatched by body heat. These
creatures then burrow into the skin (my sandal-clad foot, your pretty face?) where they
feed and grow just under the skin. After several months they reach maturity, painlessly
squeeze out, and fall to the ground to continue their life cycle.
- Diagnosis is by a mosquito bite that doesn't go away. After several weeks it
resembles a boil, except for a tiny hole in the center. If you look closely with a
magnifying glass you will see something pushing to the surface every so often to breathe
and expel waste. (Yes, the botfly larvae breathes through its butt.) As it feeds it
occasionally delivers a sharp pain like a hot needle stabbing into flesh,
which lasts only a few but very long seconds.
- Treatment is simple, if you know how. You cannot just squeeze it out as the beefworm is
ringed with barbaric barbs which tightly hold flesh. And since the beefworm produces its
own antibiotic to prevent infection while alive and healthy, you don't want to rip it
apart as an infection would likely develop. The traditional Mayan method is to pour
tobacco juice into the hole, which kills the beefworm in about an hour. You then easily
squeeze it out.
- Another method which worked for me is to suffocate the beast overnight by covering the
hole with multiple layers of Elmer's glue and plastic wrap. It becomes poppable if you
manage to cut off 100% of its air. On the second try mine flew several meters through the
lower atmosphere before smashing into an obstruction.
- Tumbu fly
- This African fly lays eggs on clothing left out to dry, which later hatch with skin
contact. Results and treatment are similar to the botfly. Prevention is by ironing clothes
to kill the eggs, or by hiring fly swatters, although this is said to be unreliable.
-
- Urine fish
- Reported in some Central American rivers to also hang on with barbaric barbs. I haven't
yet determined whether urine fish are fact or of the same class as the Amazonian ear
weevil, which renders victims insane from otherworldly pain as it bores from one side of
the head to the other. (See a medical professional before developing world travel!)
Hydraulic Currents and General Lessons
How to Avoid Insect Bites
The best way to avoid malaria and over one-hundred other mosquito and insect-borne
diseases is to avoid being bitten in the first place. Since only some insects are disease
carriers, you vastly reduce your chance of infection by limiting the number of bites.
Furthermore, it may take more than one bite from a disease-carrying insect to transmit
disease.
The first line of defense is long sleeves and pants. In jungle areas I'm much more
comfortable wearing loose-fitting cotton pants and a long-sleeved cotton shirt. They are
plenty cool and dramatically reduce every kind of insect bite. Note that mosquitoes can
slide their proboscises through a knit or too-thin shirt. Light colors such as khaki are
less attractive to mosquitoes.
The second mosquito defense is DEET (diethyl-meta-toluamide). This is
a powerful (it melts some plastic) insect repellent recommended and used world-wide. While
the FDA is currently investigating possible side-effects in children, it has stated the
benefits of DEET far outweigh these side effects, which are likely to be minor. Indeed,
not contracting malaria and other insect-borne diseases is priceless.
DEET repellent should be applied following the manufacturer's instructions to all
exposed skin. Do not apply it under clothing. Many travelers also apply DEET to sleeves,
collars, socks, and cuffs to further discourage bugs.
 Some DEET products consist of a
100% formulation for maximum effectiveness of up to eight or ten hours. 3M makes Ultrathon,
a 33% DEET product with a special carrier which slowly releases the DEET for a claimed
effectiveness of up to twelve hours. Ultrathon is also absorbed less through the skin,
thus making it safer than 100% DEET. The CDC recommends formulations from about 25 to 35%.
Some DEET products consist of a
100% formulation for maximum effectiveness of up to eight or ten hours. 3M makes Ultrathon,
a 33% DEET product with a special carrier which slowly releases the DEET for a claimed
effectiveness of up to twelve hours. Ultrathon is also absorbed less through the skin,
thus making it safer than 100% DEET. The CDC recommends formulations from about 25 to 35%.
I've used Ultrathon in a tube with good results. Many health care professionals
recommend it. It also comes in a spray can with a 23% formulation which lasts up to eight
hours, and is better for sensitive skin. The tube is lighter and lasts longer.
I reapply a little Ultrathon cream every few hours while hiking since all DEET products
lose effectiveness as you sweat.
Other Mosquito Defenses
 Permethrin is an effective repellent which is only approved for
application to clothing and mosquito netting, not skin. It is considered safe when used in
this manner. Permanone, Coulstan's Duranon, and Sawyer are brand
names of permethrin aerosol spray marketed as tick repellents. One good spray treatment
lasts several weeks. Coulston's Perma-Kill 4-Week Tick Killer is a liquid which
lasts four weeks on clothing, longer on mosquito netting.
Permethrin is an effective repellent which is only approved for
application to clothing and mosquito netting, not skin. It is considered safe when used in
this manner. Permanone, Coulstan's Duranon, and Sawyer are brand
names of permethrin aerosol spray marketed as tick repellents. One good spray treatment
lasts several weeks. Coulston's Perma-Kill 4-Week Tick Killer is a liquid which
lasts four weeks on clothing, longer on mosquito netting.
Mosquito netting is essential for sleeping in the tropics. It drapes around your bed or
hammock from a hook or line strung above it. While many hotels in the tropics lack
screens, they often have fans which produce enough breeze to prevent mosquitoes from
landing. Unfortunately, you can count on electric power regularly going out.
Mosquito netting with too-fine mesh can be stifling. On the other hand if the mesh is
too coarse black flies and no-see-ums can penetrate. Spraying or soaking mosquito netting
in permethrin dramatically increases effectiveness. Store the net in a plastic bag to keep
the permethrin effective longer. Be certain there are no gaps or holes in the netting
around you, and that no part of your body rests against it, as mosquitoes are seriously
bloodthirsty. Make sure there are no mosquitoes already inside the netting.
Mosquito head nets may also be useful. I used one while summer camping in Norway where
the mosquitoes were frighteningly monstrous and multitudinous. (Two could whip a dog,
four could hold down a man and butcher him--Mark Twain.) Head nets alone are not
enough in malarial areas, though.
Mosquito coils are spiral-shaped candles that repel mosquitoes and other bugs with the
natural chemical pyrethrum. They burn for several hours, and are useful when cooking
dinner while camping, or in hotel rooms without screening. Cintronella is another natural
repellent adequate for backyard use in the States, but not effective in serious biting
insect areas where efficacy is vital.
Insects are also attracted to scents, so don't wear perfume or cologne, or use scented
soaps, shampoos, or deodorants. Unscented deodorants are available. Several women have advised that Avon's Skin So Soft lotion fends off
minor backyard flying insects in the U.S.
Mosquitoes do not attack as long as you walk at a fair pace, or if there is a breeze.
They wait for the wind to calm, the electricity to shut off, or for you to fall dead from
exhaustion.
Cuts, blisters, and other wounds can become infected very fast in the tropics due to
the rich microbial environment. Great care must be taken to thoroughly clean wounds, and
to treat with an antiseptic such as tincture of iodine, which is good because it also
kills viruses. Keep wounds covered with a clean bandage and recheck. Double-strength
triple antibiotic ointments such as Neosporin are also helpful.
Rashes
To combat itching from stings and plants in the tropics, be sure to have antihistamine
pills and a tube of 1% hydrocortisone anti-itch cream. After two mysterious, expanding red
rashes appeared on the back of my leg, you can bet I'll never again travel in itch country
without serious anti-itch medication.
I may have crushed a poisonous millipede between my calf and thigh. While I didn't feel
anything, I noticed two small, elongated black spots which looked like burns. I
should have immediately irrigated with water and wiped with alcohol to remove as much
poison as possible. Instead I ignored the situation for two days. Gradually the poison
expanded about three inches beyond the initial sites, creating two purple and red, excruciatingly
3 itchy rashes. By scratching I
transferred poison to other parts of my body.4
Calamine lotion was next to useless. Benadryl antihistamine pills worked well. I later
discovered 1% hydrocortisone cream also works well. There is a new Benadryl cream which is
probably effective.
Plants and stings that cause nasty itching are a surprisingly effective and common
defense. The best counter-defense is always a layer of clothing and shoe leather.
If afflicted take immediate action by washing the affected area with water, beer, or
spit. Run water over it for ten or more minutes if possible. (For a cobra sting
run it
all night.) Then disinfect with soap or alcohol. Again, in the tropics you
risk infection by scratching severe itches.
Foot Care and Blisters
This is probably the #1 backpacker health concern. Have a thick pair of socks such as
Thorlo in your pack in case blisters develop. Also, at the very first sign of a "hot
spot," take action. Don't trudge on doing more damage than necessary. Allow the
healing process to begin sooner on something not so bad, as opposed to later on worse.
I keep a piece of Compeed, a great blister product, in my wallet, more in my
pack. When you do get a blister it may be miles to the nearest pharmacy, which is too far,
too late. Duct tape, Moleskin, and a liquid product called NuSkin also work.
Blisters become easily infected in the tropics, so be extra careful to avoid them, and
keep them clean and disinfected when they develop. If you decide to pop a blister, use a
sterilized needle and apply antiseptic. Cover and check regularly.
I also have a 1/3 ounce (10 milliliter) plastic bottle of Lotrimin AF
(clotrimazole) antifungal solution in my medical kit to treat fungal infections. (I just
noticed the use-by date has expired.) An effective antifungal is necessary to treat
athlete's foot, ringworm, and other unusual skin infections which may crop-up during
extended tropical travels.
Effects of the Sun
In rural Mexico I came across an Austrian traveler who had been wandering three weeks
without hat or sunblock. He was as red as a beet, and obviously dazed from
excess solar radiation. Weakly pointing to my straw cowboy hat, he mumbled, "That's what
I need..."
The sun is very intense in the tropics and at higher elevation. For every 5000 feet
(1500 meters) in altitude gain, UVB radiation increases by twenty percent. Travelers
should wear a hat with at least a three-inch brim all around, and use sunblock with a sun
protection factor of at least fifteen.
Sunglasses with ninety-nine percent UVA/UVB protection will be much desired by the
hitchhiking traveler, and protective goggles are a must for preventing snowblindness at
altitude.
Heat and Humidity
In one to three weeks the body gradually acclimates to heat through a physiological
process. Unacclimated travelers run a risk of heat exhaustion or heat stroke if they try
to do too much, too soon.
 |
If you are AC-addicted or from a cool climate, use caution and
allow time--soon the
hot environment will seem cooler. Knowing your body is adjusting should be a comfort. |
| Photo: Here I'm jungle trekking and
drinking six quarts per day. |
Travelers may be able to partially acclimate themselves to a hot environment like Egypt
by taking daily saunas for a week or two before departure, gradually building exposure
levels.
High humidity is the worst aspect of the tropics for many travelers. Wear loose cotton
clothing and drink lots of clean water. A wet bandanna around your neck or forehead
provides good cooling.
Prickly heat is a red rash which occurs under clothing. I've had it a few times on my
legs before becoming acclimated. It has a moderate prickly feeling, and goes away after a
day or two. Prickly heat is assuaged by cool showers, cold water sponging, calamine
lotion, and loose-fitting, breathable clothing. In my case clothing should also be
well-rinsed of detergent, which is harsh in developing countries.
- Heat exhaustion
- is caused by overexposure to heat by a non-acclimated person, or insufficient water or
salt intake by any person.
- Symptoms include fatigue, dizziness, nausea, headache, and possibly muscle cramps.
Treatment consists of rest, shade, and drinking water at a slow but steady rate, including
water with a weak salt solution of approximately 1/4 teaspoon per eight-ounce (1/4 liter)
glass. Cool the body with water, wet towels, and a fan, if possible. If the victim becomes
unconscious, feet should be raised twelve inches above the head.
- After twelve miles of jungle hiking in one day--half with a pack--I suddenly realized I
had heat exhaustion as I had stopped sweating and was beginning to feel nauseated. I had
drunk several liters of water that day, but that was far from enough. Luckily I was only
half a mile from camp (I was on a night hike), so I immediately returned and slowly drank
two more liters of water. I had moderate nausea and chills, and felt terrible. In the
morning I was much better and drank several more liters.
- Heat stroke
- follows untreated heat exhaustion. It often results in rapid death due to a breakdown of
the body's heat regulating mechanisms. Body temperatures can reach soaring levels.
- Symptoms usually include a cessation of sweating; shallow breathing; hot, dry, and
flushed skin; unconsciousness; and if conscious, disorientation or stupor.
- Treatment must be immediate. The victim should be placed in shade and his body cooled as
quickly as possible. Remove all clothing and wrap him in wet towels, or sponge the body
continuously with cool water. Direct a fan at the victim. If unconscious, raise feet
twelve inches. If conscious, give the victim water, preferably with 1/4 teaspoon salt per
eight-ounce (1/4 liter) glass. Medical help must be summoned.
- Hypothermia
- is a life-threatening condition defined as body temperature below 95º F (35º C).
Temperatures do not have to be extreme to cause hypothermia, since water and wind can
combine to rapidly chill a person. Most deaths from hypothermia occur in well-above
freezing temperatures.
- Symptoms include a pale, drowsy, confused, and cold victim. She may become unconscious.
Treatment consists of seeking immediate medical help and warming the victim. Warm drinks
are effective, as well as hats, blankets, emergency aluminum blankets which reflect body
heat, and, of course, warm shelter. Remove wet clothing.
- Prevention is by wearing warm clothing in insulating layers, a windproof/waterproof
shell, and a hat. An aluminum reflective space blanket should be in every traveler's pack.
Avoid cotton clothing in cold, wet conditions.
- Frostbite
- must be treated immediately by warming affected areas. Massage is not helpful, but
placing feet and hands under armpits is. If warm water is available, place the affected
areas in it. The water should not be hotter than 110º F (43º C). Remove constricting
clothing, rings, and watches. Don't warm affected areas with direct heat, such as from a
lighter. Don't allow someone to walk on a frostbitten foot, unless it's necessary for
survival.
Altitude sickness is also called acute mountain sickness (AMS). It occurs when
ascending to altitude before the body has time to adjust to the lower air pressure and
lower oxygen content of the air. It usually occurs at altitudes above 8000 feet (2500
meters). About twenty-five percent of travelers to high altitudes will be affected, but
younger people are more susceptible.
Symptoms are usually mild and flu-like, such as headache, shortness of breath,
dizziness, nausea, and fatigue. Insomnia often results due to shortness of breath. Usually
these symptoms last only a short time as the body adjusts. Many travelers have trouble
sleeping their first night or two in high altitude cities such as Quito, Ecuador (9350
feet or 2850 meters).
Severe cases result in fluid buildup in the lungs. This leads to intense
breathlessness, coughing and wheezing. Fluid may also build-up in the brain, leading to
severe headache, seizures, vomiting, hallucinations, and even coma.
Treatment for mild cases is usually just rest. Plan for an easy day or two upon landing
in Quito. Aspirin may help. Avoid alcohol and drink plenty of fluids. Locals drink coca
tea to alleviate symptoms. It acts as a mild stimulant and pain killer.
Treatment for severe cases requires immediate action--if you wait until morning the
victim may die or suffer brain damage. She should be brought down at least two or three
thousand feet and have oxygen administered. She should also be brought to a hospital as
soon as possible where diuretic drugs may be given.
Prevention is best by slowly gaining altitude. If you walk to gain altitude you can go
back down a few thousand feet if you begin feeling symptoms. One rule of thumb is to
always sleep below the highest altitude achieved that day.
Motion Sickness
If you are susceptible to motion sickness, Dramamine pills work better if
taken before symptoms develop. Scopolamine ear patches may also help. While at
sea or riding a bus get as much fresh air as possible, and focus vision towards the
horizon--not the chicken cage next to you. Think pleasant thoughts. Avoid greasy or spicy
foods. During an attempt to earn travel money on the Bering Sea my bargemates and I ate
crackers to alleviate queasiness.
Jet lag isn't much of a problem for most backpackers. We don't have to be up for an
important meeting at a certain time, and for the first few days can simply rest when we
need to. Our internal clocks adjust to the new sunlight and social schedule within a few
days. Traveling east, say from the Americas to Europe, takes a slightly longer adjustment
period since you must begin sleep earlier to synchronize with the environment. Traveling
west mainly requires staying up extra late. Jet lag is more of a problem for anachronistic
Chinese leaders experiencing democracy and rule of law for the first time/people on
speeding bus tours.
Note that airplane air is extremely dry (one or two percent humidity), so on transocean
flights drink plenty of fluids to avoid partial dehydration on your very first day.
Backpackers' Medical Kits
Right now in my pack I have a quart-sized plastic zip bag I call a medical kit. It
consists of a few band-aids, larger bandages, and butterfly closures; a few yards of cloth
tape wrapped around a pencil; a one-ounce dropper bottle of iodine antiseptic; a 1/2 ounce
(15 milliliter) tube of triple antibiotic ointment; an unopened bottle of Potable Aqua water
disinfectant tablets;  Compeed blister pads; a 1/3 ounce (10 milliliter) bottle of
Lotrimin AF antifungal solution; a 1/2 ounce tube of Cortaid 1% hydrocortisone anti-itch
cream; aspirin; a thermometer in a taped-shut plastic case; tweezers; twelve Immodium
tablets; ten chewable Pepto Bismol tablets; ten antihistamine pills; twelve Ciprofloxin
antibiotic capsules as prescribed by my travel clinic; a packet of rehydration salts; and
144 condoms.
Compeed blister pads; a 1/3 ounce (10 milliliter) bottle of
Lotrimin AF antifungal solution; a 1/2 ounce tube of Cortaid 1% hydrocortisone anti-itch
cream; aspirin; a thermometer in a taped-shut plastic case; tweezers; twelve Immodium
tablets; ten chewable Pepto Bismol tablets; ten antihistamine pills; twelve Ciprofloxin
antibiotic capsules as prescribed by my travel clinic; a packet of rehydration salts; and
144 condoms.
Additional medical items elsewhere in the pack are small folding scissors;
one-a-day-type vitamins; duct tape; a small piece of Compeed or Moleskin in my wallet; and
a four-ounce bottle of rubbing alcohol which I use for disinfecting hands when soap and
water isn't convenient.
Before my next trip to the developing world my travel clinic will prescribe a
combination of anti-malarial pills, another antibiotic, and possibly a sterile syringe and
needle.
Outdoor shops and catalogers sell pre-assembled medical kits that range in price from
$8 to over $100. They don't contain doctor-prescribed antibiotics or medicines. I've
always assembled my own. See Chapter 23-b Useful Information
for two companies that specialize in medical kits.
Upon Returning Home
If you come down with an illness soon after returning from the developing world, inform
your doctor of that fact. Many tropical diseases are very difficult to diagnose, and mimic
the flu. You may need to see a tropical disease specialist. You may also want stool and
blood tests to see if anything unusual is lurking about. Otherwise wait two years
to see if your stool becomes bloody and lower intestine blocked by a gigantic mass of
ascaris lumbricoides, or other.
Travelers' Tips
Make a notecard of your medical history and keep it in your wallet. Indicate
whether you have any known food and drug allergies, and any known health conditions. Also
your blood type, and any other instructions. Several companies, such as Medic-Alert, make
bracelets and chains which also contain this information. Aida, Brooklyn
*
Beware of salads, especially lettuce, in developing countries with suspect water
supplies. The rule is if you can't wash it, peel it, or boil it, don't eat it. Lisa,
Christchurch, New Zealand
*
When we arrived in Sri Lanka and engaged a driver with car we
insisted on having a car with seat belts....We may owe our lives to this because after ten
days our driver went off the road and down a six metre drop into a culvert. We were
wearing belts and so--for the first time--was our driver. We all walked away...thankfully
with no serious injuries. Andrew, UK
*
My schedule will be drastically compressed if the test comes back positive in five
and a half months. Turbo, USA
How to See the World is copyright © John Gregory 1995-2009. All rights reserved. Except
for personal use like showing to a friend, it may not be reproduced, retransmitted,
rewritten, altered, or framed. All
product names and trademarks are property of their respective
owners. Comment.
Sales.
Disclaimer. Thank you.
............
.
|
|
. |
. |
....... .
. |
.. |
.. |
. |
.`
|
| ....... |
:)
. |
. |
. |
..... |
.. |
.. |
. |
. |
| . |
. |
|
. |
. |
. |
|
. |
. |
| . |
|
. |
. |
...............
. |
. |
. |
|
. |
| |
. |
. |
. |
......................................... . |
. |
. |
. |
|
| ......
.............. |
. |
. |
. |
ARTOFTRAVEL.COM
.
|
. |
|
(: |
..
.
.
......... . |
| . |
. |
. |
. |
. |
. |
. |
. |
. |
Notes
1. My rough calculation: 50,000 automobile deaths per year x 70 year
lifespan = 3.5 million total deaths. 350 million projected population ÷ 3.5 million =
100, or a 1 in 100 chance. back
2. After a years-long night and first light filtered through the front of
the bus I cried out to myself, Thank God! We're there! But nay, it was five
hundred miles and many mountains, many mountains to go. back
3. Chosen over torturously, because in uncivilized countries that's a
lifetime punishment for thinking and speaking. back
4. O to learn. back



 Some DEET products consist of a
100% formulation for maximum effectiveness of up to eight or ten hours. 3M makes Ultrathon,
a 33% DEET product with a special carrier which slowly releases the DEET for a claimed
effectiveness of up to twelve hours. Ultrathon is also absorbed less through the skin,
thus making it safer than 100% DEET. The CDC recommends formulations from about 25 to 35%.
Some DEET products consist of a
100% formulation for maximum effectiveness of up to eight or ten hours. 3M makes Ultrathon,
a 33% DEET product with a special carrier which slowly releases the DEET for a claimed
effectiveness of up to twelve hours. Ultrathon is also absorbed less through the skin,
thus making it safer than 100% DEET. The CDC recommends formulations from about 25 to 35%. Permethrin is an effective repellent which is only approved for
application to clothing and mosquito netting, not skin. It is considered safe when used in
this manner. Permanone, Coulstan's Duranon, and Sawyer are brand
names of permethrin aerosol spray marketed as tick repellents. One good spray treatment
lasts several weeks. Coulston's Perma-Kill 4-Week Tick Killer is a liquid which
lasts four weeks on clothing, longer on mosquito netting.
Permethrin is an effective repellent which is only approved for
application to clothing and mosquito netting, not skin. It is considered safe when used in
this manner. Permanone, Coulstan's Duranon, and Sawyer are brand
names of permethrin aerosol spray marketed as tick repellents. One good spray treatment
lasts several weeks. Coulston's Perma-Kill 4-Week Tick Killer is a liquid which
lasts four weeks on clothing, longer on mosquito netting. 
 Compeed blister pads; a 1/3 ounce (10 milliliter) bottle of
Lotrimin AF antifungal solution; a 1/2 ounce tube of Cortaid 1% hydrocortisone anti-itch
cream; aspirin; a thermometer in a taped-shut plastic case; tweezers; twelve Immodium
tablets; ten chewable Pepto Bismol tablets; ten antihistamine pills; twelve Ciprofloxin
antibiotic capsules as prescribed by my travel clinic; a packet of rehydration salts; and
144 condoms.
Compeed blister pads; a 1/3 ounce (10 milliliter) bottle of
Lotrimin AF antifungal solution; a 1/2 ounce tube of Cortaid 1% hydrocortisone anti-itch
cream; aspirin; a thermometer in a taped-shut plastic case; tweezers; twelve Immodium
tablets; ten chewable Pepto Bismol tablets; ten antihistamine pills; twelve Ciprofloxin
antibiotic capsules as prescribed by my travel clinic; a packet of rehydration salts; and
144 condoms.